SURGERY FOR DIABETES – where are we now?
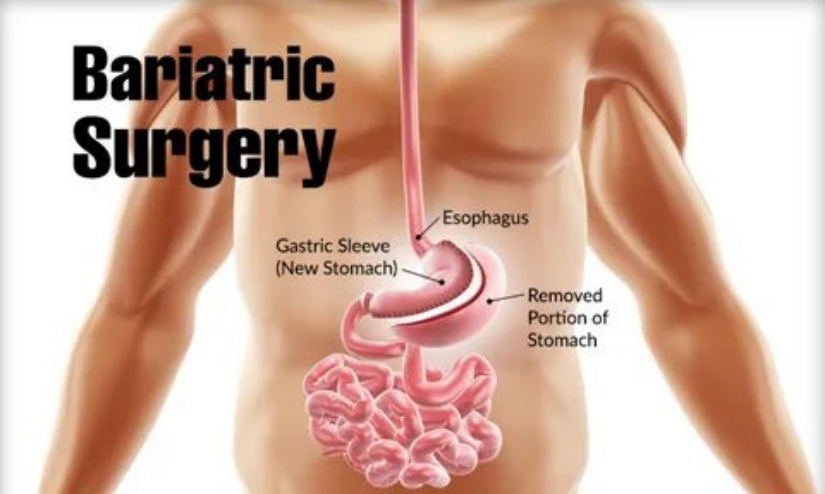
Obesity has grown at a rapid pace in the last few decades. While diet and activity remains the mainstay treatment, the efficacy of this modality for morbid obesity is very low. Bariatric surgery has proven to be the most effective treatment for morbid obesity. This produces significant and durable weight loss. Further, it leads to significant resolution, remission, or improvement of obesity related diseases such as diabetes, dyslipidemia, hypertension, sleep apnea, arthritis, polycystic ovaries and fatty liver.
Although the effect of bariatric surgery on mechanical complications such as arthritis is understandable, the effect of bariatric surgery on diabetes is particularly interesting. The improvement in blood sugar levels appear immediately after bariatric surgery much before any significant weight loss has taken place.
This positive effect was also seen in the low BMI individuals. In a study by Panunzi et al, the efficacy was shown to be similar in patients with BMI < 35 and > 35. This finding has led surgeons and researchers to explore the interesting possibility- can we reverse/ remit type 2 diabetes, so far known to be a chronic progressive disease?
This exciting work has led to development of a new branch of science and terminology- “metabolic surgery”. Currently, the term is applied to GI surgery when its primary intention is to treat metabolic syndrome especially type 2 diabetes including patients with mild obesity.
Various mechanisms have been proposed and studied that go beyond weight loss to improve hyperglycemic status. It has been hypothesized that there is an increase in gut hormones (incretins) due to altered gut anatomy. This leads to insulinomimetic action and improved diabetic status. One incretin called GLP-1 has been studied extensively and shown to increase after surgery in various studies. Not surprisingly, GLP analogues are also used by physicians for diabetic control. The rapid contact of nutrients to distal intestine either due to duodenal bypass and hyper motility called “foregut and hind gut hypothesis” have been proposed as the reason behind the elevated GLP-1. Other gut hormones that have been studied and known to contribute to glycemic control are GIP and PYY. Other mechanisms that may contribute to glycemic control after surgery are – alteration in gut microbiota, change in bile acids and intestinal glucose sensing. These factors have all been under a lot of attention and a subject of intense research.
There are various metabolic procedures. For almost a century, surgeons knew that gastrectomies, gut resections and gastrojenunostomy improved glycemic status. Bariatric procedures producing benefits for diabetics are also a serendipitous finding in science. In terms of efficacy, Duodenal switch is the best procedure for diabetes control. However, because of the high incidence of malnutrition, it is not popular amongst surgeons. Gastric bypass has been shown to be better than sleeve gastrectomy in many studies. Recently, One anastomosis gastric bypass (OAGB) demonstrated superior efficacy over conventional gastric bypass.
Inspired by the success of metabolic surgery and the concept of duodenal bypass for glycemic control, there has been various endoscopic innovations. Endoluminal Barrier Device and Duodenal Mucosal Resurfacing are two such exciting options that are being developed in this field.
The support for metabolic surgery comes from a vast published literature in the last 3 decades. In one of the landmark papers published in 1993 titled provocatively as “Who would have thought it! – A surgery proves to be the most effective therapy for type 2 diabetes”, Dr Walter Pories showed excellent results in his cohort of diabetic patients. Many authors have subsequently published their encouraging results on the subject. There are now more than 15 RCTs that demonstrate superior efficacy of metabolic surgery over medical therapy for type 2 diabetes. These trials show that the median HbA1c drops by 2% for surgery compared to 0.5% with conventional therapy. Further, metabolic surgery reduces the chances of macrovascular complications. Some benefits in microvascular complications have also been reported. This is a huge advancement in clinical care for diabetes.
Despite the large body of evidence in favour of metabolic surgery, there has not been a proportionate increase in its incorporation for the treatment of diabetes.
There are some reasons behind this. Critiques argue that these studies are short to medium term and no long term data exists. Newer anti diabetics such as those that work via renal glycosuria produce better weight loss and needs to be compared with surgery. Further, there is attrition of beneficial effects from surgery with time. Like any other GI surgery, metabolic surgery comes with its complication rates. There is a short-term complication of about 2% and long term nutritional issues which requires lifelong supplementation and monitoring. Therefore, a diabetic patient should know the trade-off when offered surgery.
These observations has led surgeons to improve on identifying patient cohorts who would benefit from surgery. It is known that diabetes is a heterogeneous disease with various sub groups. It is possible that there are some who respond better than others. Data analysis has led to understanding predictors for surgical outcome. Short duration of diabetes, younger age, high C-peptide levels, and mild diabetes respond better to the surgery. These predictors have been incorporated into scoring systems such ABCD and Diarem. They may help in improving outcomes in future.
The pathophysiological reason proposed behind improved outcomes with better scores is that those with low beta cell reserves, typically seen in long standing diabetes, do not respond well to metabolic surgery. Hence, there is a suggestion to use metabolic surgery in early disease.
Overall, it is clear from
published literature that metabolic surgery gives improved results over medical treatment in medium term, and possibly preventive benefits on macrovascular and some microvascular complications. Therefore, metabolic surgery should be a part of treatment algorithms for diabetes.
However, metabolic surgery should be done in tertiary centers where multidisciplinary treatment is offered. Diabetes Surgery Summit II recommends metabolic surgery for patients with BMI > 40, and BMI 35-40 patient with uncontrolled diabetes. In these cohorts, the benefits are clear. It also proposes that it should be “considered” for diabetic patients with BMI 30-35.
Clearly, more research is needed to answer questions. It is important to define the cohort of diabetics where metabolic surgery would work optimally. The physiological mechanisms of glycemic control need to be better understood. The risk-benefit ratio and cost effectiveness will have to be defined. Filling these knowledge gaps are essential in developing the field of metabolic surgery.